A Visionary Solution to Dry-Eye Syndrome
Mike Lovett
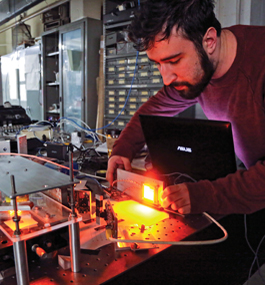
Dave Matthews '18 makes adjustments to a Schlervey test model.
by Lawrence Goodman
Physicist Hermann Wellenstein spends a lot of time thinking about what happens when subatomic particles smash together at nearly the speed of light. A member of Brandeis’ high-energy physics group, Wellenstein and his colleagues conduct research at the Large Hadron Collider, near Geneva, Switzerland.
But when Wellenstein’s late wife, Monika ’85, was suffering from lupus, the physicist turned his gaze toward a very concrete problem. As a side effect of the autoimmune disorder, Monika developed dry-eye syndrome. Wellenstein began to look for ways to make treating the condition less uncomfortable for her and other patients.
Dry-eye syndrome can damage the eye’s surface, creating ridges, bumps, rough patches and gaps. To treat it, Monika needed scleral lenses, similar to contact lenses but large enough to cover most of the sclera, the white outer region of the eyeball. The lenses form a seal with the sclera, creating a chamber that can hold saline solution or other fluids. The liquid bathes and lubricates the eye surface, providing relief from burning, itching and blurred vision.
But a scleral lens must form a perfect seal to prevent the liquid from escaping. And the eye is not a perfect sphere. Wellenstein watched his wife undergo the discomfort — and sometimes pain — of repeated fittings, as the ophthalmologist searched for the right lens shape. It took days to get the fit right. As her disease progressed, Monika needed to be refitted for lenses several times.
“I was always asking the doctors if there was something I could do to help,” says Wellenstein.
Although he was not able to develop a solution in time to help his wife, Wellenstein is now putting the finishing touches on Sclervey, a system to survey the sclera so patients with dry-eye syndrome and other corneal diseases can be fitted for lenses more efficiently. Two undergraduates — Forrest Webler ’14 and Dave Matthews ’18 — played major roles in developing Sclervey.
“It was just incredible to work on something that has real-world applications and can change people’s lives,” says Matthews.
The Sclervey is a concave dish, which is placed about four inches from the patient’s eye. The dish is divided into segments shaped like pizza slices, each containing a panel of roughly two dozen LED lights. When the lights go on — they are dimmer than a cell-phone screen so they won’t damage the eye — cameras positioned around the dish photograph the eye, capturing the location of the light spots projected onto the sclera. Changes in the sclera’s contours alter the light spots’ positions.
To interpret the data, Wellenstein and his students needed software that could map the photos generated by Sclervey into a 3-D image of the sclera. The software would have to detect variations between the points of light as small as 50 microns, about half the width of a human hair.
This is where Wellenstein drew on his experience at the Large Hadron Collider.
When protons traveling at close to the speed of light are smashed together inside the collider, a set of new subatomic particles are released. Wellenstein and his colleagues developed software that monitors the detectors that trace the pathways taken by the new particles.
It turns out that the same software is able to analyze the patterns of light spots in the pictures taken by Sclervey’s cameras. Indeed, the device detected differences as small as 15 microns. Next, it created a 3-D image of the sclera that, in theory, an ophthalmologist can use to create a scleral lens. Instead of resorting to trial and error, doctors should be able to create a perfect fit the first time out.
The next big step? Wellenstein and his lab hope to find a partner, possibly a nonprofit, to begin clinical testing on humans.