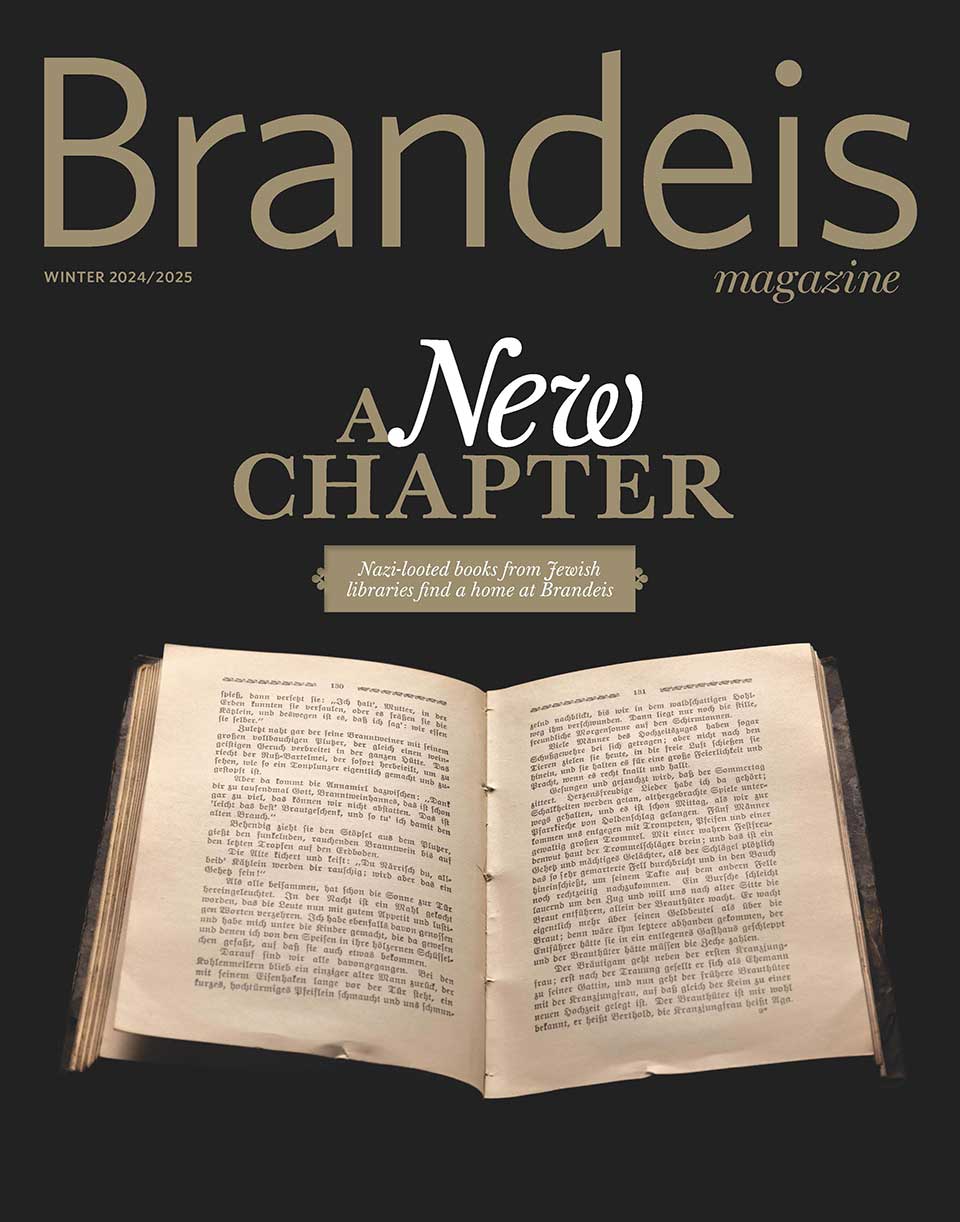
Walking Toward a Good Death
A new book by Brandeis anthropologist Anita Hannig reveals how medical aid-in-dying can restore dignity and a sense of control to those facing terminal illness.

James Steinberg
Anita Hannig is an expert on how we die.
A medical and cultural anthropologist who studies life’s bookends — birth and death — she’s the author of “The Day I Die: The Untold Story of Assisted Dying in America” (Sourcebooks, 2022), a moving portrait of individuals who overcome formidable barriers to plan and carry out a medically assisted death.
In a style more journalistic than academic, Hannig takes readers inside bedrooms, living rooms and courtrooms to explore the complicated issue of medical aid-in-dying in the U.S., and observe the empowerment that can come as the terminally ill assume control of their death.
Over hundreds of hours, she shadowed patients, families, lawmakers, activists and physicians. She worked as a hospice volunteer and was a firsthand witness to several planned deaths in Oregon, which legalized medically assisted dying in 1997, the first state in the nation to do so.
Not surprisingly, Hannig became emotionally involved in her research. And though she didn’t start out as a committed advocate for assisted dying, she became one. “You can’t do this research and not be swayed one way or another,” she says. “I couldn’t attend these deaths and remain unmoved.”
For many Americans, medically assisted death remains shrouded in stigma, misunderstanding and taboo, despite the fact that nine states and Washington, D.C., have joined Oregon in enacting assisted-dying legislation over the past 25 years. Today, one in five Americans has legal access to an assisted death. Seven in 10 Americans say they support assisted dying, according to a 2020 Gallup Poll. “Yet we live in a death-phobic society,” says Hannig, who, at 40, is an associate professor of anthropology, a new mother and a serious athlete.
Her book never loses sight of the big questions: How do the dying gain agency over death? What is medicine’s role at the end of life? How do we restore dignity to death in our high-tech age, when the chasm between the living and the dying seems ever-widening?
Hannig believes easing restrictions on aid-in-dying laws is a good place to start. For example, U.S. laws, which are more restrictive than those in other parts of the world, require the dying person to self-administer a lethal pharmaceutical cocktail — an impossibility for many patients with terminal illnesses that make swallowing difficult, such as Lou Gehrig’s disease. Physicians should be allowed to administer lethal medications to those who otherwise meet the aid-in-dying criteria, Hannig says.
In addition, assisted-dying laws require that two physicians determine a patient is in the last six months of life — a narrow time frame that’s difficult to predict, and one that excludes terminally sick people who experience unbearable suffering earlier in their illness.
“An assisted death is not the easy way out,” Hannig writes in “The Day I Die.” “Hastening the end of your life is an act of will that demands improbable courage. It means accepting the hard truth of your mortality and walking toward death with clear, open eyes.”
In the book excerpt that follows (reprinted by permission of the publisher), Ken, a 90-year-old husband, father and grandfather, is suffering from congestive heart failure, aggressive prostate cancer and a leaky heart valve when he decides to end his life with the help of Oregon’s medical aid-in-dying law.
Hannig prepares to go to his home to witness his death.
The morning of Ken’s death, I stood in front of my closet, trying to figure out what to wear. I knew Ken didn’t want his death to be a somber affair. He was ready, giddy even. The drab librarian dress was definitely out. Jeans, on the other hand, seemed a little too casual. I wanted to look nice and give Ken’s death the gravity it deserved, while also honoring his wish to celebrate. As I thumbed through my hangers, I couldn’t help but feel the dissonance of choosing an outfit for someone’s final hours. Three years into my research on assisted dying, I still found myself in situations like this with no formal playbook. But if I didn’t decide promptly, I was going to be late. Finally, I opted for a pair of striped summer slacks, a sleeveless, navy blue satin blouse, and leather sandals. Then I grabbed my notebook and ran out the door.
Thirty blocks to the east, at the foot of one of Portland’s iconic city parks, Ken was also getting ready. Though he had spent much of his life flouting propriety, he had decided to dress up for his death. In the quiet light of the morning, he trimmed his white Van Dyke beard, slipped into a clean pair of khakis, buttoned his olive-colored dress shirt and threw on a charcoal vest. He dug out his red bandanna and tied it in a neat triangle knot around his neck. Then he traded his tired plaid house slippers for a pair of elegant, pointy leather brogues.
Ken’s breakfast that day was simple: a single hard-boiled egg and a cup of black coffee laced with Fireball whiskey. Not that it was his habit to drink alcohol with breakfast — it didn’t mix well with his heart medications — but today Ken felt festive. He had waited for this day for months.
At 10:30 a.m., I met Ken’s prescribing physician, Neil Martin, in the foyer of Ken’s retirement facility. Save for his medical bag, which could have passed for a plump briefcase, you wouldn’t have guessed Martin was a doctor — he wore a cornflower-blue dress shirt, black Levi’s and hiking sneakers. Martin had begun working with terminally ill patients interested in using Oregon’s Death with Dignity law in 2009. After his retirement from family medicine in 2015, he had kept his license so he could continue to volunteer as a physician.
Martin and I signed the facility’s guest log and made our way to Ken’s apartment in the far corner of the building. At the entrance to the dining hall, next to a roster of activity charts announcing bingo night and water aerobics, a cluster of walkers sat parked, waiting for their owners to return. We swung a left down a wide hallway lined with rustic watercolor paintings all depicting stone bridges reaching across gurgling creeks. The pictures conjured a pleasant but generic nostalgia. Ken couldn’t stand them.
When we entered his apartment, everyone else was already there: Ken and his two sons, Tony and Zack; Ken’s granddaughter, who had flown in from California; and Sophie, his beloved caregiver. Standing and chatting among the family was Derianna Mooney, a volunteer for End of Life Choices Oregon — a nonprofit that accompanies patients and families on their path to an assisted death. Derianna was here to ensure that everything went smoothly and that Ken felt supported in his wish to die.

David Neff
Anita Hannig
page 2 of 3
The apartment looked exactly like it had the last time I was there: stuffed with furniture, unwieldy plants, Ken’s hand-drawn paintings and stacks of loose paper. Two golden helium balloons — spelling 90 — still clung, bloated, to the ceiling like giant bubbles trapped under a bottle cap. Ken had turned 90 exactly a week ago.
In the years leading up to his 90th birthday, Ken had gone from living in a house in Southern California he shared with his wife, Clara, to living with her in a sheltered but intolerably dull retirement complex in Portland, to living alone after he had to admit her to a memory care facility. Worried about their dad’s declining health and their mom’s progressive dementia, their sons had persuaded Ken and Clara to sell their house near San Bernardino and move up to Portland to be closer to them. For the first six years after their move, Ken had taken care of Clara himself in their shared one-bedroom apartment inside the retirement complex, but eventually Clara required specialized help. The physical separation from his wife hit Ken hard — they had been together for over 60 years.
In the beginning of Clara’s stay at the memory care facility, Ken visited her four times a week. But for the past few months, he had needed to cut back on his visits.
“I’m running out of gas. It’s a real big deal to make it up the hill,” he told me during one of our talks, gesturing to the slope between his patio and the parking lot.
Ken no longer drove, but he let his caregiver, Sophie, chauffeur him in his old Toyota Camry so he could go see Clara. Sophie had recently procured a wheelchair for Ken, but he hadn’t wanted to use it yet. “I hate to have to be wheeled in there to see Clara. So I tough it out, but geez, it’s getting tougher and tougher.”
Ken couldn’t be sure if his wife recognized him anymore.
“She’s getting really, really bad. It’s getting iffy now if she even knows me when I go over to visit. But I still go.”
By the time Ken went for his final visit a few days after his 90th birthday, Clara’s Alzheimer’s had long made her unable to process or communicate information, so there wasn’t much in the way of a formal goodbye. But Ken believed that Clara would have supported his decision to hasten his death. When they were younger, they’d had many philosophical talks about their end-of-life wishes. Ken was convinced that he had his wife’s blessing.
As I greeted his family, Martin, Derianna and Ken huddled to go over some last-minute logistics. I could tell that something was off. Ken’s voice sounded hoarser than usual, and a look of panic flared in his eyes. Martin hadn’t remembered that Ken had a pacemaker until just now. He thought it would be safer to turn it off prior to Ken’s death to prevent it from jolting him back to life after his heart stopped beating.
Turning off a pacemaker falls under the responsibility of a cardiologist, which meant that Ken would have to postpone his death. Martin stepped into the bedroom to make some calls.
Ken chastised himself. He had been so careful to put all the pieces in place. Two days ago, he had called Derianna late at night to ask if he should still take his heart medications on the day of his death. He didn’t need to, she had said. He also wanted to know which foods to avoid to maximize his body’s absorption of the lethal dose. “Nothing too fatty,” she had advised, so no steak the night before. And now this.
Minutes later, Martin reemerged with the good news: The pacemaker could remain on. Unlike other pacemakers, Ken’s didn’t have a defibrillator, so it wouldn’t interfere with his plan to die. Ken heaved a sigh of relief and lowered his tall frame into his armchair. His dog Fluffy, a white shih tzu, jumped onto his lap. Smiling broadly, Ken folded his veiny hands around her. He locked eyes with Martin, who nodded and stepped closer.
Kneeling in front of Ken so they could be at eye level, Martin held a bottle of Seconal, a powerful barbiturate, between his thumb and index finger. It had Ken’s first and last name written on the label.
“Do you know what this medication will do to you, Ken?” Martin asked. The question was part of a protocol the doctor followed each time to ensure that a patient fully grasped what was about to happen.
Ken lifted his eyebrows and puckered his lips. He was gearing up for a joke. At the last moment, he thought better of it. Ken sat up straight.
“I will never wake up again.”
“Do you still want to proceed?” Martin needed to know.
Ken couldn’t resist.
“Well, I wouldn’t want to chicken out now. The party’s already in full swing, and all the guests are here.”
page 3 of 3
Martin rested his mocha eyes on Ken, waiting patiently, studying his face. There was a tenderness in the doctor’s mannerisms that surprised me every time I saw him interact with a patient. What I had initially mistaken as shy reserve was a deep and abiding empathy for human hardship. I sometimes wondered if he had chosen medicine or if medicine had chosen him. Martin told Ken that it wasn’t too late for him to change his mind. They could call the whole thing off right now, Martin said evenly.
A sense of alarm flashed across Ken’s face.
“No, I want to go through with it,” Ken said, holding the doctor’s gaze. He sounded more sincere now, more resolute.
Their exchange reminded me of a similar conversation I had with Ken about a month ago. I had asked him if he thought he might change his mind when it came closer to the end. He had stared at me with a firmness I had never seen in him before.
“No! Not me. If we’re gonna rob a bank, we’re gonna rob a bank, OK?”
At the time, I broke into a grin and thought, I would rob a bank with you. I liked Ken. Some people probably found his sense of humor grating, but to me his candor felt refreshing. Even at 90, Ken didn’t let anyone put him over a barrel. But he also knew that not everyone shared his sense of relief that his life would soon be over.
“I have to respect the kids, too,” he had said to me. “I don’t want to try to make a happy occasion out of what they think is a sad occasion. But I think they’re realistic about it.”
Ken’s sons knew about their father’s daily physical struggles. How numbness crept up his arms. How fluid retention caused his limbs to inflate. How he had started urinating blood. How every time he exerted himself, he would experience a piercing pain in his chest. How he could barely walk the 50 feet to the parking lot outside his back door — even with the assistance of a walker and Sophie’s help — without feeling like he was having a heart attack.
“I’m getting worse every day,” he had told me, the weary look in his eyes amplified by his droopy eyelids and tinted glasses. “I don’t want to have a stroke and have the boys take care of me and my wife. I’m more afraid of living than I am of dying.”
— Anita Hannig
Later that morning, Ken sat on the side of his bed. His family gathered around him. Hannig, Martin, Mooney and Sophie looked on from the doorway. A blues song Ken had written and recorded played in the background. Soon after drinking a lethal Seconal cocktail, Ken drifted into a deep sleep. He died within 10 minutes.
Find Hannig at anitahannig.com and on Twitter at @AnitaHannig.